Embryo genetic testing as a part of IVF is complicated so I will explain CGH embryo testing and other options . CGH stands for Comparative Genomic Hybridization and is microarray testing. The confusing part is that it is sometimes called Comprehensive Chromosome Screening (CCS). Both of these (CGH or CCS) are the newer and better technology to in situ hybridization (FISH), that is commonly referred to as traditional Preimplanation Genetic Diagnosis (PGD).
What is Comparative Genomic Hybridization (CGH)?
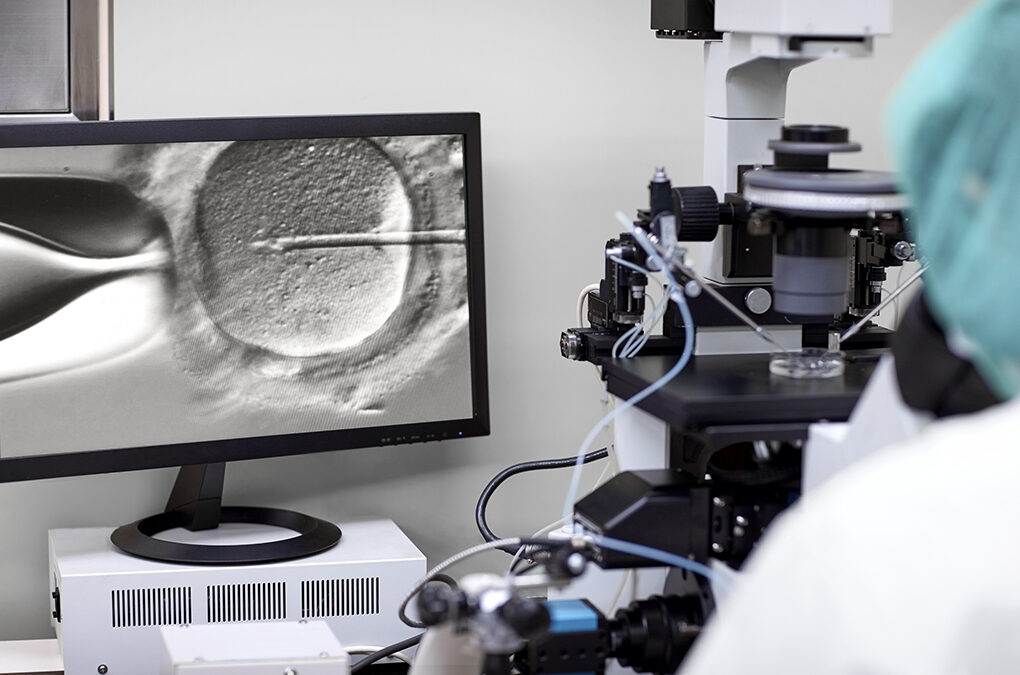
CGH is advanced chromosome screening for embryos. It determines whether or not the embryos are normal, allowing you to pick the best ones for transfer. Abnormal embryos (Aneuploidy) are the cause of more than 60% of miscarriages. In the normal course of IVF, embryos are graded just by looking at them under the microscope, however abnormal embryos often look just like normal embryos. What this means to me, is that microscopic embryo grading is pretty much useless and means that you’re flying blind when picking the embryos. Therefore, CGH can help you increase your chance for pregnancy and live birth.
Hopefully soon, this type of testing will be used in most all IVF cycles and will become standard.
CGH/CCS is a great option for women who:
– are 35 or older
– have a history of repeated miscarriages
– had a previous pregnancy involving a chromosomal abnormality
– have had multiple failed IVF cycles
CGH vs. FISH (PGD)
| What is tested? | Chromosomes? | Average Cost | |
| CCS or CGH | 5-10 cells of Day 5 Blastocyst | 23 pairs of chromosomes (all) | $4000-$6000 |
| PGD or FISH | 1-2 cells of Day 3 Embryo | 5-11 chromosomes | $3500 |
Advantages of CGH Embryo Genetic Testing
Ability to Pick the Best Embryos: For women 35 and older with day 5 transfers, 1 out of every 3 embryos are aneuploid (abnormal). After embryo grading using the microscope, a decision is made on which embryos to use. After CCS, usually that decision changes in 40% of cases. To me, this is staggering. For example, a friend of mine had a perfect-looking 5AA embryo that they would have transferred. Then, they did CCS testing and discovered that that embryo was abnormal with a trisomy 18, changing their decision on which embryos to transfer.
Tests all chromosomes: There’s a lot less chance for error when more cells are tested and every chromosome is looked at. FISH testing has a chance for false negatives, while CCS is more accurate.
Less Damage to Embryo: Biopsying the embryo at a more advanced cell stage dramatically increases the accuracy of this testing and minimizes potential damage that the biopsy can cause on the embryo because it has several hundred cells by then.
Better Chance for Singleton Pregnancy: CCS gives doctors the knowledge that they are transferring the most chromosomally fit embryo, therefore precluding the need to transfer multiple, unscreened embryos in the hope that one will be healthy enough to create a pregnancy and a healthy baby. Pregnancy rates are the same for transferring one CCS-tested embryo vs. two non-tested embryos.
Better Birth Rate: Using FISH with IVF does not increase birth rates, however using CCS does.
Disadvantages of CGH
One potential disadvantage is that you must have day-5 blastocysts to utilize this technology. For some couples, I imagine this is problematic. Also, I think you would probably want to have at least 4 embryos to test to make it worthwhile.
Also, the embryos must be frozen because the embryos can’t survive outside the body to Day 7 to wait for the results of the testing. So, they are flash-frozen using vitrification, which is a newer and better method to traditional cryopreservation. Cryo usually has about 65-75% survival rate with about 50% cell loss. Vitrification has 90% survival rate with almost no cell loss. Because of the new freezing technology used, we didn’t feel that this was much of a disadvantage.
The CGH/CSS embryo testing process
– Egg Retrieval
– Fertilization using ICSI which is necessary to prevent contamination with residual sperm adhered to the egg when they do the biopsy.
– Embryos grow in the lab
– Biopsy done on day-5 blastocysts
– Biopsies were transported to the testing lab and then vitrified at our lab.
– Results in two days from the lab, pick embryos.
– Ready for a frozen transfer (FET).
Why we decided to do CGH testing
Ultimately, we decided to do the testing because we didn’t want to have any regrets and because some doors opened for us with the costs. Even though we had every reason to believe that the problem lies with my body, we also had no proof that our embryos were healthy. They looked good under the microscope, but that doesn’t necessarily mean anything. We were solving the problem with my body by using a gestational surrogate, but we also wanted to guard against any possible problems with the embryos by doing this testing. We wanted to give ourselves the best chance possible with the surrogate. After 7 years, 6 IVFs and 5 miscarriages…this was it – our last shot! We had to go all in and not hold back.
I felt that CGH would give me peace of mind that if I got pregnant, I would have a higher chance of a normal baby. I was really worried about birth defects ever since hearing my friend’s results because she had a perfect embryo they were going to use and then testing revealed it to be a Trisomy 18. So, birth defects are on my radar. There was NO reason to think this would be a problem for us, but after the incredibly difficult journey, we just wanted to be extra careful and give ourselves the best possible outcome.
The biggest downside was that I needed more aggressive treatment to get enough eggs to be able to make enough 5-day embryos. Even when I’m treated conservatively, I still got OHSS. So, I had to go into it knowing I might get it again, but I did not!
We want to eliminate any possible problems because we wanted no regrets, less stress in worrying about it and because that cycle was going to be our last shot.
My embryo testing results
Out of six embryos tested, we had four normal or euploid embryos and two abnormal or aneuploid embryos. That was great news for us!
They told us to expect half of them to be aneuploid, so we beat the odds!
We are so glad we did the testing! Of the six embryos, we had four highly graded embryos at grade 8 (the highest) and two fair-graded embryos at 5. The two abnormal embryos were two of the highly graded ones. Therefore, selecting them for a transfer would have resulted in a 50/50 shot of getting one of the abnormal ones.
Here’s what the results look like
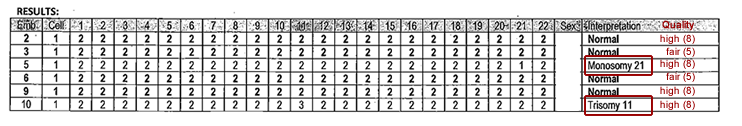
The info on the left is the CGH microarray testing. The info in red on the right is the basic microscopic embryo grading.